Tongue Ties, Lip Ties, Cheek Ties... Oh My!
You’re feeding your baby. Or trying to. And something just feels... off. Maybe it’s pain, clicking, shallow latching, endless feeds, or a gassy, frustrated baby. Maybe someone casually mentioned tongue tie. Maybe you’re deep in a late-night Google spiral trying to figure out if your baby’s frenulum is too short or too thick or if something else might be going on.
As an IBCLC, I’ve been in the trenches with hundreds of families trying to figure this out. So let’s take a deep breath and get honest, evidence-based, nuanced about oral restrictions.
What Is a Tongue Tie?
All humans have a frenulum under the tongue. A tongue tie (ankyloglossia) is when that tissue is short, thick, or tight enough to restrict movement of the tongue — and that restriction is interfering with function. That’s the keyword here: function. It doesn’t matter how dramatic it looks. If your baby can feed well, speak well, eat well, and breathe well, it's probably not a problem.
Babies can also have:
- Lip ties: the frenulum connects the upper lip to the gum too tightly
- Buccal (cheek) ties: less common, but some believe they may restrict cheek movement
These ties are made of connective tissue that doesn’t stretch on its own.
Posterior Ties: The Hidden Ones
Posterior tongue ties attach further back on the tongue blade and can be hidden behind layer of mucosa. You might not see them as obviously as a more "anterior tie" which causes the visible "heart-shaped tongue"— but they can still cause major issues. A baby may appear to have a “normal” tongue at a glance but still struggle with mobility and latch. Posterior ties tend to impact the LIFT of the tongue, which can have major impacts on feeding function. Infant many families don't release that is it is LIFT of the tongue that matters most in breastfeeding mechanics and not tongue extension - that is why EVEN if your baby can extend their tongue, they still can have a tongue tie.
'According to Dr. Gaheri one of the leading researchers on tongue tie and it's impact on feeding.
"A posterior tongue tie is the presence of abnormal collagen fibers in a submucosal location surrounded by abnormally tight mucous membranes under the front of the tongue. A classic anterior tongue tie always has a posterior component behind it. Therefore, any tongue tie causing breastfeeding problems is truly a posterior tongue tie; a percentage of those ties also have an anterior component. Failure to release all of the abnormal collagen fibers results in persistent tongue restriction"
This is why a quick clip in the pediatrician's office or during your hospital stay may not have been adequate. - The ANTERIOR portition of the restriction was released, but not the full tongue tie and the baby can still struggle with feeding.
Signs That May Point to a Tie
- Painful nursing for the parent (bleeding, cracking, blisters, creases on the nipple)
- Clicking or popping during feeds
- Milk dribbling from lips
- Swallowing air / frequent spit-up (take a look at the video below for a demo)
- Shallow latch or slipping off the breast
- Short, inefficient feeds or super long, exhausting ones
- thick white coating on the tongue from the tongue not resting up on the roof on the mouth
- Weight gain concerns despite frequent nursing
- Constant feeding / cluster feeding that never ends
When It's Not a Tongue Tie
Here’s the thing: not every feeding struggle is caused by a tongue tie. I know TikTok and Facebook groups might make it feel like “tie” is the answer to every problem — but real life is a little more complex than that.
Lots of babies show signs that look just like a tongue tie, but actually have something else going on. And that’s why jumping straight to a release — without a full assessment — often leads to frustration.
So what else could it be?
Feeding is a full-body experience. Your baby’s ability to latch, suck, and swallow well is connected to more than just the mouth. Many babies are born with body tension — from being curled up in the womb, from a tough birth, or just from how they’re wired. You might see side preferences, tight necks or shoulders, or crooked body posture. And guess what? Tight muscles can absolutely impact feeding mechanics.
On the flip side, some babies are born with low tone — meaning their muscles are a little floppy and don’t hold tension well. Feeding takes a lot of coordination, so low tone can make sucking feel like a marathon. These babies may benefit from things like cheek or jaw support and very intentional positioning to help them feed more effectively.
Even if you’re already working on body tension or tone, sometimes the feeding issues stick around. That’s when we might dig deeper and say, “Okay, is there also a tongue tie here getting in the way?” For example, a baby’s gassiness may improve with therapy — but they’re still struggling to transfer milk or losing milk out the sides of their mouth. In that case, it’s time to look again and reassess.
Bottom line: not every baby with symptoms has a tie. But every baby with symptoms deserves a thorough, function-focused evaluation. And parents deserve real answers — not quick dismissals or rushed snips.
Why Function > Appearance
Some babies have the classic “heart-shaped” tongue tip but feed like champs. Others look normal but are miserable and not transferring milk. Function is everything. The tongue should:
- Elevate fully to the palate
- Extend past the lips
- Move side to side (lateralize)
- Cup around a finger or nipple
If those skills are restricted, it can absolutely affect feeding — breast or bottle.
This is a clip of a functional oral assessment feeling around the mouth and accessing tongue mobility, strength and tone.
What About Lip and Cheek Ties?
Lip ties alone rarely cause feeding issues unless paired with a tongue tie. The lip needs to be able to be in a neutral but not rolled-in position at the breast, but it doesn’t play the same role in milk transfer. However, lip ties can:
- Make latching tricky
- Cause milk dribbling
- Contribute to cavities later if brushing is painful
Cheek (buccal) ties are even more controversial. Some say they restrict oral function, others argue they’re being overdiagnosed. Evidence is limited, but if your baby has inefficient sucking and poor cheek seal, a cheek tie could be part of the puzzle.
My clinical experience echo's that of Dr. Gaheri quoted below:
" In my experience, if a baby comes to my office with breastfeeding problems and has a tie, 99% of the time that child will have a tongue tie. They may also have a lip tie (about 50-60% of the time) accompanying the tongue tie but isolated lip tie is very uncommon - it makes up less than 1% of the babies that I treat. Those few babies have normal tongue function; the lip restriction is the only obstacle to achieving a normal latch. For most babies, however, a tongue restriction is the problem. - Dr Bobby Gaheri Tongue tie vs lip tie: which is more to blame?"
The Process: What To Do If You Suspect a Tie
Here’s the ideal process (not just snip and hope):
- Start with a lactation consultant (IBCLC) to assess latch, milk transfer, and feeding mechanics.
- Get a bodywork eval (CST, PT, OT) if baby has signs of tension or asymmetry.
- Work on oral motor function (sometimes with an SLP or OT trained in infant feeding).
- If ties are suspected and symptoms persist, get a referral to a release provider (dentist or ENT who specializes in ties).
- Do pre-op exercises to prep the tongue/lips to move post-release.
- Have the release (frenectomy) with a trusted provider who uses scissors or laser.
- Follow with aftercare and therapy — so baby learns to use their new range of motion.
Why do you do to prepare for a release?
If it’s determined that your baby has signs of tongue, lip, or cheek ties, your care team (usually a lactation consultant, SLP, or OT) should guide you through the whole process — not just the release, but everything before and after too. Because here’s the deal: a tongue tie release (frenectomy) isn’t a quick fix. And it’s definitely not the right move for every baby.
That’s why hitting all the right steps in the right order matters. A good provider won’t just look at the mouth — they’ll be checking for body tension, oral motor skills, feeding patterns, and looking at the family system as a whole. If you are recovering from a traumatic birth, dealing with postpartum OCD and your baby is very tense THIS IS NOT THE IDEAL TIME FOR A RELEASE!
If your baby has tension patterns that impact jaw, head, or body movements, they may refer you to someone trained in bodywork — like a physical therapist, occupational therapist, chiropractor, or craniosacral therapist.
And sometimes? That bodywork is enough. Releasing tension alone may fully resolve your baby’s symptoms — no scissors or lasers needed. Other times, it makes a big dent in the issues and clears the way for a better release (if one is still needed).
Your therapist will also help you figure out timing — because this isn’t a same-day thing. A typical release process is 6+ weeks start to finish. That includes preparation (so the tongue knows how to move once freed) and follow-up (so those new movements stick).
Let me say this clearly: Getting a tongue, lip, or cheek tie release without therapy is unlikely to give you the results you’re hoping for. Your baby needs to build the skills to use that new range of motion, not just have the tissue snipped.
A tongue tie release IS NOT AN EMERGENCY. You need to be prepared, regulated and supported going into the process.
The Tongue Tie Process
- Start with a functional assessment by an IBCLC who is educated in ties- they may pull in an OT or SLP or PT, depending what other challenges exist.
- Do bodywork with a professional trained in tension patterns — like a PT, OT, chiropractor, CST, or IBCLC with special training to help you prepare for release.
- If needed, consult with a release provider (usually a pediatric dentist or ENT)- talk to the IBCLC you are working they will have recomendations just don't go with the provider you can get in with soonest - and unfortunatly you may need to travel or pay out of pocket to see the most experiences release provider.
- Begin oral motor therapy to help build tongue, lip, and jaw strength.
- If ties are still impacting feeding, move forward with the release (frenectomy).
- Start wound care and post-op stretches as recommended by your release provider- more why this is important below.
- Continue therapy and feeding support - the release is usually not a quick fix and we want to make sure baby is learning how to use this new mobility correctly and not just reverying to old compensation patterns.
Why does after-care of the wound matter?
I love this quote from Dr. Gaheri one of the top researchers in tongue tie outcomes in breastfed kiddos. "When a provider creates a wound in the mouth to try and release a tethered band, the mouth will try close that wound. In the context of tongue tie and lip tie, we want those wounds to heal in an open conformation rather than closed back together....Remember, once an open wound is created in the mouth, the body will try to close the wound and contract toward its center. The end result is that the lip will try to stick back down to the gumline and the tongue will try to stick back down to the floor of mouth. The trick to achieving optimal results is to try and guide the tissue, through proper stretches, to heal in a way that maximizes vertical movement."- Dr Gaheri
Aka your body is smart and want's to heal things as soon as possible and we don't encouage the wound bed to heal in a open postiontion that will allow the tongue to lift in the most effective way. If this is unclear head over to Dr. Gaheris blog he has some great illustrations.
I love this quote and image from Shondra Mattos IBCLC
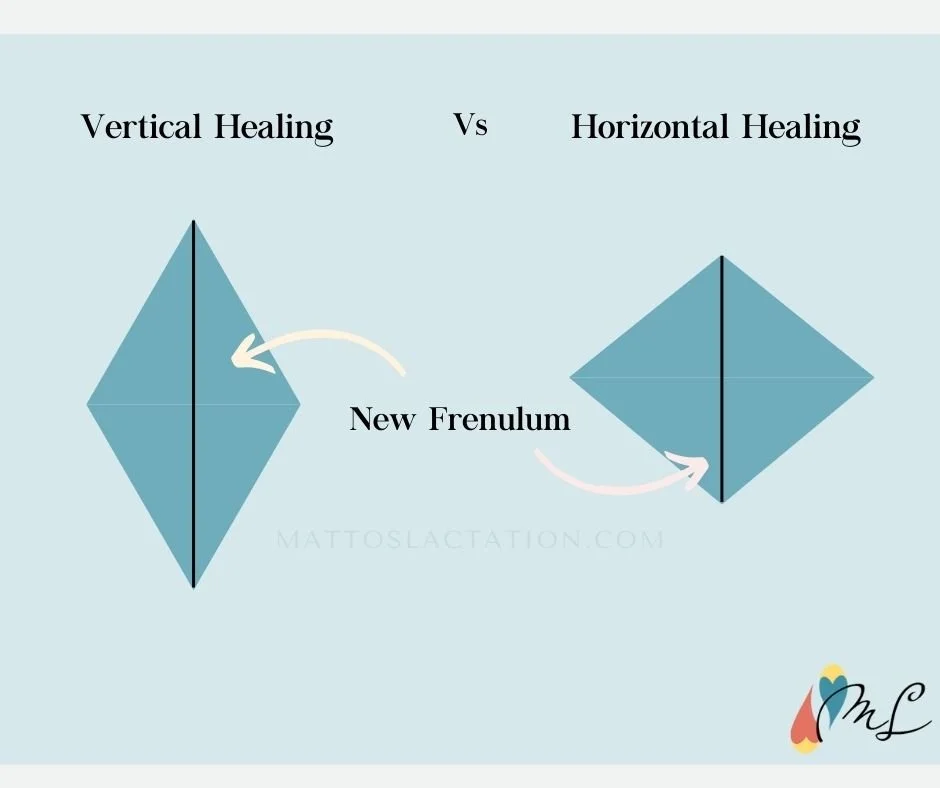
"When the wound heals slow, long & tall, there is more time & space for a longer frenulum to form. Compare that to a wound that heals short & flat with the edges of the diamond healing downward toward each other in the same orientation as before the release."
But Are Ties Over-diagnosed?
Whew — big question. The short answer? Sometimes, yes. Sometimes releases are done too soon, without the prep work or time to try less invasive strategies first. And sometimes… ties are completely missed.
The truth is, many pediatricians aren't trained to assess ties functionally. Some providers jump straight to a release that wasn’t really necessary. Others totally dismiss valid concerns, leaving families feeling gaslit and stuck. The system? Kinda messy.
That’s why you need a team — an IBCLC, a feeding therapist, and a release provider — all looking at the same baby, through the lens of function, not fad.
We’re not chasing perfect-looking tongues here. We’re looking for movement. Comfort. Milk transfer. Growth. Relief. In other words: function over appearance, always.
What About Bottle-Fed Babies?
Tongue ties affect bottles, too. You might see:
- Gulping or coughing during feeds
- Milk leaking out the sides
- Loss of suction / need to reposition constantly
- Gas, spit-up, or choking
- Trouble pacing
Sometimes, bottlefeeding masks the issue because it's easier than nursing. But if symptoms persist, it's worth investigating. I have absolutely worked with exclusively bottle fed babies who needed a release to be able to feed effectively. This little baby in the video is a great example - hear the clicking? see the milk leaking?
Just because a baby is bottle-fed doesn’t mean feeding challenges don’t matter — or that they’re easier to spot. In fact, bottle feeding can mask issues like poor suction, tongue restriction, or low tone because the flow is more passive. But if your bottle-fed baby is leaking milk, gulping air, coughing, constantly losing the latch, or feeding feels stressful… that’s worth investigating. Every baby deserves a feeding experience that’s comfortable, functional, and supportive — breast, bottle, combo, donor milk, formula, all of it.
Do Tongue Ties Cause Long-Term Issues?
Untreated oral ties can impact:
- Speech development
- Breathing (mouth breathing, snoring, sleep-disordered breathing)
- Jaw and facial growth
- Eating skills
- Dental health
But again, only if they’re actually causing functional problems. Not every tongue tie leads to lifelong issues. That’s why the assessment matters so much
Why does tongue posture matter
Your baby’s mouth posture might not seem like a big deal, but it’s actually the foundation for how they’ll breathe, eat, and eventually talk. The position of the tongue plays a huge role here — it’s not just hanging out in there doing nothing. The tongue helps shape the mouth as your baby grows. Think of it like a natural palate expander (way cooler and gentler than the orthodontic ones later). A nice wide palate gives your baby more room to breathe through their nose and function like the little human they’re becoming.
So what are we looking for?
At rest — meaning your baby isn’t eating, crying, or cooing — the tongue should be up against the roof of the mouth, and their lips should be gently closed. The tongue tip should rest just behind the upper gum ridge. This is what we want to see most of the time. If their mouth pops open occasionally while snoozing or spacing out? Totally fine. But if their mouth is constantly hanging open, or their tongue always seems low or forward, it might be worth a second look.
Noticing these things early gives you a head start. Because when we support optimal tongue posture now, we’re setting the stage for easier feeding, clearer speech, and even better sleep down the line.
The Resting Tongue Check
Want to see where your baby’s tongue likes to hang out? Here’s a quick little check you can do (no medical degree required):
First, take a peek while your baby is resting or sleeping. Is their mouth closed and peaceful? Or is it open like they’re mid-yawn... all the time?
If your baby’s mouth is frequently open at rest — especially during sleep — it’s worth paying attention to. When the mouth is open, the tongue can’t be resting up against the roof of the mouth, and that often means baby is mouth breathing. This can mess with feeding, sleep, and even oral development over time. If you’re also hearing noisy breathing or snoring sounds in a newborn (yep, even little baby snores), it’s a good idea to chat with an airway-savvy specialist.
Now for the quick at-home check:
👉 While your baby is sleeping or super relaxed, gently place your finger under their chin and softly try to close their mouth. Hold it closed for about 5 seconds and watch what happens. Do they keep it closed? Or do they pop it right back open?
Then, take your index finger and gently pull down on their chin to open their mouth slightly. Look inside: is their tongue staying up toward the palate? Or does it drop down like it’s clocking out for the day? That little tongue position can tell us a lot. And if it seems consistently low, it may be part of the bigger picture when it comes to feeding, airway, or oral development
What to do to help improve resting tongue posture in your baby
So you’ve noticed your baby’s mouth is often open at rest, or their tongue seems to hang low. First of all, you’re not doing anything wrong. And no, your baby isn’t broken. But there are some things you can do to gently support better tongue posture — because tiny shifts now can make a big difference over time.
1. Gently close the mouth
Gently use your finder to press up behind your baby's chin in the fleshy part (practice on yourself to feel how this manuever lifts the tongue). This should help suction the tongue to the roof of the mouth- if the mouth immeaditly drops back open over and over and you are having other red flags its time to reach out to tongue tie savy provider.
2. Tummy Time Is Your Friend
Tummy time isn’t just about neck strength — it also supports whole-body alignment and helps activate the muscles that lift and stabilize the tongue. Even a few minutes at a time, multiple times a day, adds up. Bonus: it helps release tension patterns that may be keeping baby’s mouth posture funky.
3. Bodywork Can Help- here is my friend Austin Rees IBCLC CST doing craniosacral therapy.

Tension in the jaw, neck, shoulders, or even hips can impact how the tongue moves and rests. Working with a pediatric chiropractor, craniosacral therapist (CST), physical therapist, or occupational therapist can help gently release tight spots and get baby’s body back in balance — which often leads to improved mouth closure and tongue lift without ever touching the tongue itself.
4. Optimize Feeding Position
Whether you’re nursing or bottle-feeding, positioning matters. Aim for a calm, aligned posture — baby’s ears, shoulders, and hips should be in a line. For bottle-feeding, use a paced feeding approach with baby held upright and the bottle horizontal. Good feeding mechanics = better oral tone and coordination = more natural tongue elevation. Check out out latching guide!
5. Support Oral Motor Skills (If Needed)
If your baby is struggling with tongue movement (especially if they're older), a feeding therapist (SLP or OT trained in oral motor therapy) can guide you through gentle exercises that encourage better tone, control, and coordination — which naturally improves resting posture over time.
6) Encourage Nasal Breathing
Babies are supposed to breathe through their noses — it helps keep the tongue up and the mouth closed. If your baby’s nose always seems stuffy, snorty, or gunky, chat with your pediatrician or a pediatric ENT. You can also use saline drops and a nasal aspirator (like the NoseFrida) to keep those little airways clear..
Can you help with a tongue tie virtually?
I’ve helped so many families navigate the tongue tie journey virtually — from those just starting to wonder “could this be a tie?” to those who were already knee-deep in the struggle. I’ve also worked with plenty of babies who clearly showed signs of a tie, even when their pediatrician brushed it off with a “no way.” Together, we’ve prepped for releases, found trusted in-person bodyworkers, tracked down preferred release providers, and made a plan — all with me supporting the family every step of the way.
Here’s the truth: not every family has access to great lactation support. In some areas, there aren’t any IBCLCs. In others, there might be some… but they aren’t trained in oral function or ties. That’s where virtual care can be a game-changer.
If you’re dealing with a suspected oral restriction and don’t have solid local support, a virtual visit with a provider who actually understands ties (hi, it’s me 👋) can still make a huge difference.
Do all IBCLCs understand tongue ties?
Honestly? No — and that might surprise you.
Tongue ties aren’t even covered on the IBCLC exam. So unless your lactation consultant has taken additional, specialized training (I’ve done, like, five courses — thanks, ADHD hyperfocus!), they probably only know the basics. That’s not a dig — it’s just the reality of the training.
And if you saw an IBCLC in the hospital? They might know something is up, but be unable to say it. Many hospitals have strict policies that prevent staff from even mentioning tongue ties unless a provider officially diagnoses it.
Can an IBCLC diagnose a tongue tie?
Nope — diagnosis is outside of our official scope of practice. But what we can do is assess how your baby is actually using their mouth and tongue, how that’s impacting feeding, and whether things are functioning as they should. If something seems off, we’ll refer you to a release provider — typically a pediatric dentist or ENT — who can give you a full evaluation and talk next steps.
What to do next if you suspect a tongue tie?
Don’t panic. Don’t feel like you have to constantly reposition your baby’s mouth 24/7. And please, don’t jump straight into a release procedure unless you’ve had a thorough, functional assessment from someone who understands oral function — not just appearance.
If you’re wondering whether your baby’s open mouth posture, shallow latch, or feeding struggles might be related to a tongue tie or something else — I got you.
🎓 Inside Boob School, we dive into exactly how tongue movement affects latch, milk transfer, and comfort — and what you can actually do to help without going down a rabbit hole of worry or getting lost in the chaos of conflicting advice.
🍼 Not ready to dive in just yet? Grab the free Latch Guide — it’ll help you support your baby’s latch and body from the start, whether you’re nursing, pumping, or combo feeding.
You don’t have to figure this out alone. And you’re already doing an amazing job. 💛


.png)
%20(13)%20(1)%20(1).png)

